West Virginia’s Kids Need Continuous Coverage
Ellen Allen
While West Virginia has done an outstanding job of getting folks the health care coverage they need, there is room for improvement when it comes to covering the state’s most precious resource — our kids.
According to a new report from Georgetown University’s Center for Children and Families on the process dubbed “Medicaid unwinding,” four out of five West Virginia children lost coverage, not because they no longer qualified, but due to administrative hurdles like lost paperwork or families not receiving notifications.
During the three years of the pandemic, states got extra money for Medicaid costs but had to agree not to cut people off the health plan. Beginning in April 2023, the federal government — which provides most funds for Medicaid — required states to resume asking people to provide proof of eligibility.
Under that requirement, families each year must provide income and other documentation to show they are eligible for the health plan for low-income children and adults.
Medicaid and CHIP income eligibility is set at a higher level for children than parents so many of the children who lost coverage during the unwinding likely still meet income eligibility guidelines even if their parents no longer qualify. The report notes that enrollment increases in separate CHIP programs only account for about 10% of the children losing Medicaid on average in those states despite earlier projections that most children losing Medicaid would seamlessly transition to CHIP.
There are reasons to worry that a high number of children are going uninsured. Being uninsured is bad for a child’s health and exposes the family to large medical bills they can’t afford. Health care can influence children’s physical and emotional health, growth, and development and their capacity to reach their full potential as adults. All children are at increased risk of developing preventable conditions if appropriate care is not provided when they are sick or injured.
West Virginia lost more than 62,000 kids, a reduction of about 11%, from its Medicaid program. However, we know that kids are being restored and we are confident in the commitment of Commissioner Cynthia Beane for the West Virginia Bureau for Medical Services to return all eligible children to coverage.
West Virginians for Affordable Health Care would like to see the state exercise options allowing for multi-year continuous coverage for West Virginia children.
States have policy options available to them to make it easier for parents to keep their eligible children enrolled: Many did just that by pausing disenrollments when problems arose, fixing their automated systems to account for differences between child and parent eligibility requirements, and increasing staffing and outreach efforts to help parents navigate the process.
Our neighboring state of Kentucky took deliberate steps to avoid cutting off children for procedural reasons as it began renewing Medicaid for adults. It is one of the few states in the nation that hasn’t seen this decline in enrollment. Kentucky Medicaid officials early on announced they would seek to protect children’s health coverage, and delayed, with federal permission, requiring children to renew coverage under the process the state began in 2023. As a result, children won’t be required to begin renewing coverage until September.
Also, Kentucky was the first state to adopt an option offered by the federal government to provide 12 months of “continuous coverage” for children and teens, guaranteeing enrollees under 19 would retain coverage for at least a year — rather than being required to renew on the anniversary of their enrollment.
Medicaid officials also launched an information blitz, with letters, calls, text messages and other means to contact enrollees to try to make sure they understood the need to renew coverage and respond to requests for information from the state.
Twelve states are planning to build on the lessons learned during the pandemic and offer multi-year continuous coverage to children with a particular focus on keeping young children insured during the critical early childhood development period between ages 0 to 6 when frequent visits to the doctor are required.
Medicaid is not a luxury. It’s a vital program for tens of thousands of children, their families and their communities, and until recently, was facing a $150 million shortfall. During the pandemic, the federal match for Medicaid was increased to help states cover the additional enrollees — West Virginia used those monies to plug various holes in state spending, leaving Medicaid funding short.
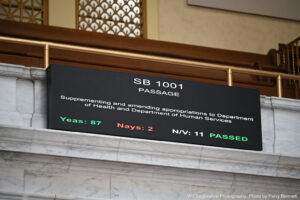
And, just under the press deadline for this commentary, West Virginia lawmakers — during the special legislative session — passed legislation to restore Medicaid funding to the governor’s original budget proposal of $183 million. However, there’s no mandate that the money has to be spent that way.
This is good news. It is encouraging. But it is not enough. It still does not adequately fund Medicaid. And it contains language that requires unspent funds to be clawed back to general revenue if not spent by March 31, 2025.
Moreover, West Virginians for Affordable Health Care urge lawmakers to pass the Managed Care Organizations tax to fully fund Medicaid into the future. There is broad support and consensus for an increase in the tax on Managed Care Organizations to address rising costs due to inflation and the end of pandemic era increased federal matching dollars.
If lawmakers fail to keep Medicaid fully funded, West Virginians risk losing access to services, health care coverage and provider stability. This would have a devastating impact on people we care about — our friends, family and communities.
It’s time for West Virginia to leverage the flexibility in options allowed under Medicaid rules to keep eligible children enrolled in Medicaid and CHIP and to reconnect those kids who were mistakenly disenrolled.
We acknowledge and thank lawmakers for restoring funding to Medicaid. Now, let’s finish the job when the Legislature meets during the August interim session.
Originally published by https://westvirginiawatch.com/2024/05/23/west-virginias-kids-need-continuous-health-coverage/